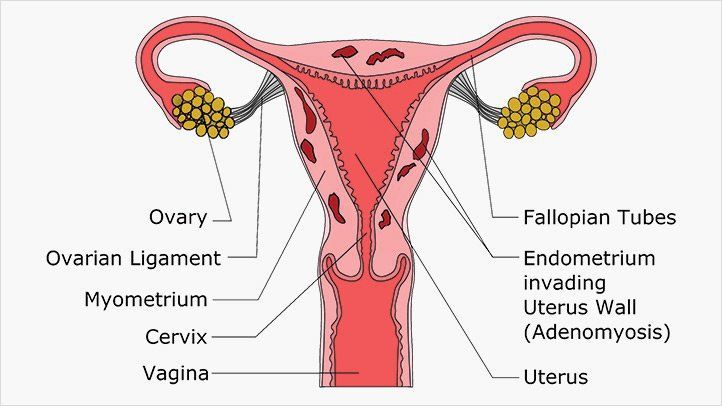
Adenomyosis is also known as endometriosis interna. Adenomyosis is a benign uterine disorder in which endometrial glands and stroma are pathologically demonstrated in the myometrium. Women affected by adenomyosis may present with abnormal uterine bleeding (AUB), dysmenorrhea, dyspareunia, or infertility but one third of them are asymptomatic. For many years, adenomyosis has remained a histopathological diagnosis made after hysterectomy in perimenopausal women with heavy menstrual bleeding (HMB) or pelvic pain. Over the last decade, adenomyosis has also become a condition identified in young fertile-age women4 thanks to the recent advancements in imaging techniques, even though a shared definition and classification are still lacking . Despite the improvement of diagnostic tools, the awareness of the condition is still poor. Furthermore, in some patients, adenomyosis coexists with other gynecological conditions, such as endometriosis and uterine fibroids6 . The physio-pathological mechanisms, involving sex steroid hormone aberrations, inflammation, fibrosis, and neuroangiogenesis, are not fully understood7 . Regarding the current management of adenomyosis, there are no international guidelines to follow for surgical or medical treatment of adenomyosis8 and this will be of utmost importance in the future as the disease requires a lifelong management plan, including pain and bleeding control, fertility preservation, and pregnancy outcome.
In fact, adenomyosis pathogenesis remains elusive and not a single theory can explain all of the different phenotypes of the disease. Furthermore, adenomyosis often coexists with other gynecological conditions, such as endometriosis and uterine fibroids, increasing the heterogeneity of available data. Treatment requires a lifelong management plan as the disease has a negative impact on quality of life in terms of menstrual symptoms, fertility, and pregnancy outcome and has a high risk of miscarriage and obstetric complications.
According to the most common theory, adenomyosis results from the invagination of basalis endometrium into the myometrium through an altered or interrupted junctional zone, which represents a highly specialized hormone-responsive structure located in the inner third of the myometrium.
Symptoms of Adenomyosis
Following are the symptoms of Adenomyosis:
- Excruciating menstrual cramps (dysmenorrhea)
- Heavy and prolonged bleeding during period
- Unable to get pregnant
- A history of early or late recurrent miscarriage
Complications of Adenomyosis: Miscarriage & Reproductive Immune Disorder
Adenomyosis can result in complications such as miscarriages and reproductive immune disorder.
Having Adenomyosis can causes changes in:
- The shape of your uterine cavity
- The uterine tissues
- The uterine blood circulation
- The local hormone levels
All the factors mentioned above can result in early and late miscarriages.
A Dilation and Curettage (D&C) procedure is usually required after a miscarriage to ensure no attachments remain inside the uterus. The D&C procedure involves scraping the uterine lining, and during the process, there is a high possibility for paternal genes to enter the mother’s bloodstream. Having paternal genes in the mother’s bloodstream will result in her body developing anti-fetal antibodies (reproductive immune disorder). Hence, you now have a reproductive immune disorder, on top of the already existing Adenomyosis. Both conditions will highly increase your chances of miscarriages.
Diagnosis
As mentioned above, Adenomyosis can cause multiples complications that will severely affect a woman’s ability to get pregnant or carry a baby to full term and lead to reproductive immune disorder. It is important to undergo examinations to ensure a proper diagnosis before getting treatment for Adenomyosis. The gold standard to make the final diagnosis of adenomyosis has always been considered histological examination of hysterectomy specimens
The examinations are:
- CA125 Blood Test. CA125 blood test can measure the local hormone levels.
- B-Scan. B-Scan can check if tissues have grown on the muscular wall of your uterus.
- Complete Blood Count. Complete blood count can check for anemia. Patients with Adenomyosis will bleed heavily during their period, and some might have anemia as a result.
- Hysterosalpingography (HSG). HSG can check for the shape of the uterus.
- Anti-fetal Antibodies Level. An anti-fetal antibodies level check can determine if you have reproductive immune disorder.
Treatment
At Antai hospital, we follow a “414 policy” when it comes to treating Adenomyosis.
We treat Adenomyosis regardless of these four factors:
- Size of the fibroids
- Number of fibroids
- Growth location of fibroids
- Age of patient
We use one effective treatment:
- We use state-of-the-art 3D-hysteroscopy surgery to remove lesions caused by Adenomyosis. Removal of the uterus is not required and not recommended.
Our four guarantees towards our patients:
- No abdominal surgery
- No removal of the uterus
- No blood transfusion (we use an autologous blood transfusion device where patients’ blood is collected and reinfused)
- No future recurrence of miscarriages
Antai’s Belief
Many doctors would recommend either hormone pills or the removal of the uterus (hysterectomy) as a treatment method for Adenomyosis. Antai strongly believes in providing treatment options for women that does not involve removing reproductive organs, unless it has become cancerous. At Antai, our team of specialists treats Adenomyosis using world-class 3D hysteroscopy equipment.