Asherman’s Syndrome: Diagnosis and Treatment at Antai
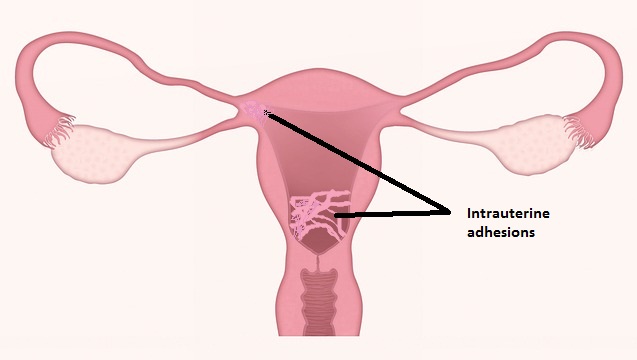
Intrauterine adhesions causing amenorrhea after curettage were first described by Fritsch in 1894. Later Asherman in 1950 described the history of 29 women with amenorrhea secondary to trauma of the uterine cavity, the Asherman’s syndrome (AS). AS is defined by the presence of intrauterine adhesions or adhesions in the endocervix with consequent risk of hypomenorrhea/amenorrhea, reduced fertility, pregnancy loss and abnormal placentation. The recently pregnant uterus seems susceptible to trauma of the basal layer of the endometrium, which can develop into intrauterine adhesions and may give future problems for the patient. It is estimated that more than 90% of cases with AS occur after pregnancy-related curettage. However, AS can develop without preceding pregnancy in cases with infection or surgery related to the uterus.
It is impossible to detect or estimate the true prevalence of all IUA, as probably most cases are without symptoms. However, the total number is irrelevant from a practical point of view. Only cases with AS, which imply pain, bleeding disorders or impaired fertility needs treatment.
Risk Factors
Trauma caused by surgical interventions, primarily curettage of the basal layer of the endometrium shortly after a pregnancy is the main reason for development of symptomatic IUA. These adhesions can result in partial or complete obstruction of the uterine cavity or the cervical canal. An incidence of 10% IUA after one curettage evaluated by HSG was seen in one randomized controlled trial. However, in women with at least two curettages 30.6% (22/72) had IUA when evaluated by hysteroscopy 10 weeks after the curettages.
Symptoms
- Infrequent or no menses
- Pain during menses, excruciating
- Infertility
- Recurrent miscarriage
Diagnosis
Several diagnostic modalities have been evaluated for the diagnosis of intrauterine adhesions (IUA). IUA can be visualized by hysterosalpingography (HSG), ultrasonography including contrast sonohysterography (SHG), 3D ultrasonography, hysteroscopy and magnetic resonance imaging (MRI). Hysteroscopy is the gold standard in studies comparing different diagnostic modalities, and several classification systems are based on hysteroscopic findings. HSG gives the opportunity to simultaneously evaluate tubal patency, but details of filling defects are not visualized, and a high false-positive rate is documented. Transvaginal ultrasonography with evaluation of the endometrial thickness in women with AS showed substantially thinner endometrium compared to normal menstruating women.
Following are the checks you can go for:
- B-Scan: B-Scan can check for endometrial thickness. The endometrium is the thickest on the 22nd day of your menstrual cycle. If you do a B-Scan on the 22nd day and it is not more than 0.8 cm/8mm, then you are considered to have a thin endometrium. B-Scan can also check for uneven endometrial thickness.
- Hysterosalpingogram (HSG). HSG can check for uneven endometrial thickness as well. It is a conventional diagnosis method for intrauterine adhesions but has slowly been replaced by hysteroscopy.
- Hysteroscopy. Hysteroscopy is now the best method to diagnose intrauterine adhesions. The scar tissues and uneven colours can be seen directly.
Treatment of Asherman’s Syndrome at Antai Hospital
Asherman’s Syndrome is treated by removing the adhesions found within the cavity or outside of the cavity. It is done via operative hysteroscopy, and upon completion, we will insert an intrauterine stent alongside with a bio-adhesion barrier to promote recovery of the endometrial lining.
Natural pregnancies can be achieved after the surgery, and it comes with a moneyback guarantee.
